Association of glutathione intake with chemotherapy resistance in breast cancer
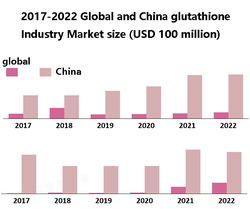
glutathione (GSH) is the most important small molecule active oligopeptide for maintaining REDOX balance in vivo.
Glutathione and related metabolic enzymes form the body's most important antioxidant defense system, protecting cells from attack by reactive oxygen species (ROS).
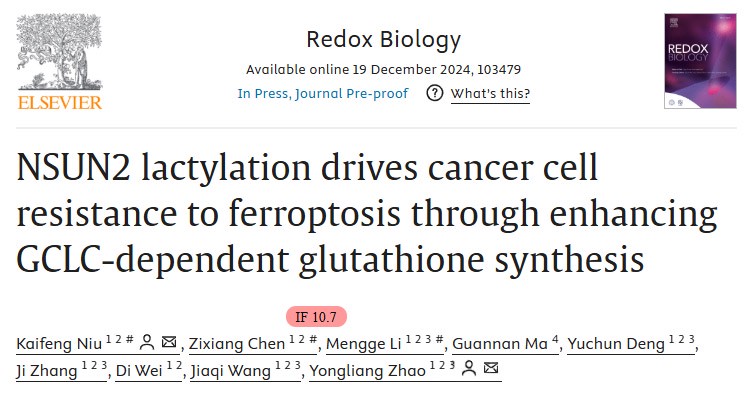
In recent years, it has been found that the level of glutathione in drug-resistant tumor cells is increased, and the expression of related metabolic enzymes is up-regulated, indicating that the glutathione antioxidant system is closely related to tumor resistance as the main cellular REDOX state regulatory system.
On December 21, 2024, Professor Wentao Li and his team from Henan Provincial People's Hospital published a paper entitled "Excessive glutathione intake contributes to chemotherapy" in the World Journal of Surgical Oncology resistance in breast cancer: a propensity score matching analysis ".
The study was designed to explore the effects of glutathione overdose on chemotherapy sensitivity in breast cancer.

The results suggest that overconsumption of glutathione may lead to chemotherapy resistance in breast cancer, and the levels of intracellular glutathione and antioxidant oxidase in resistant patients after neoadjuvant chemotherapy are increased, suggesting that regularized glutathione intake may help reduce chemotherapy resistance.
Breast cancer is the most common malignancy in women worldwide. Despite significant advances in diagnosis and treatment, the prognosis for breast cancer patients remains unsatisfactory.
The main treatments for breast cancer include surgery, chemotherapy, radiation therapy, endocrine therapy, and targeted therapy.
Treatment options are usually based on cancer stage, tumor characteristics, molecular subtypes, immunohistochemistry, and the overall health of the patient.
Although 80% to 90% of patients are eligible for surgery, 30% to 40% of patients will inevitably experience recurrence and metastasis.
10% to 20% of patients may be considered unsuitable for surgery at the time of initial treatment.
To improve outcomes, approximately 60-80% of patients require adjuvant chemotherapy and neoadjuvant chemotherapy to reduce the risk of recurrence.
There are still a large number of patients who show primary or secondary resistance to chemotherapy drugs, leading to poor prognosis.
In recent years, tumor prognosis scores at Royal Marsden Hospital (RMH) have shown potential as an important tool for assessing patient outcomes, but reliable indicators for predicting relapse and mortality after chemotherapy resistance remain scarce.
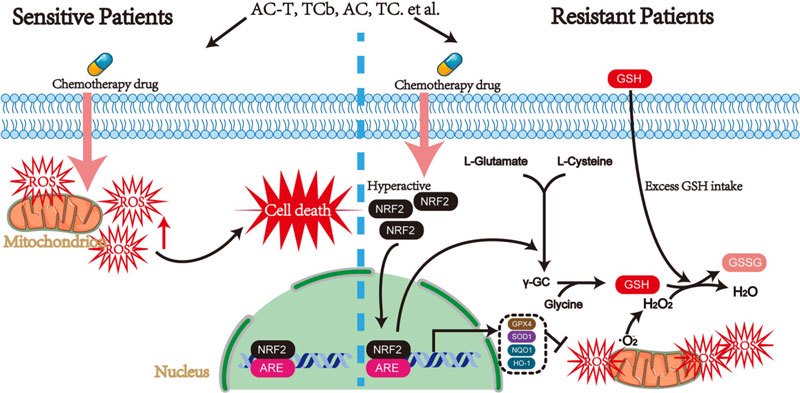
Chemotherapy-induced apoptosis has been recognized as the main mechanism of killing tumor cells. Chemotherapy promotes ROS production, which triggers apoptosis and damages tumor cells as well as healthy cells.
In response to oxidative stress-induced damage, tumor cells up-tune their antioxidant defense systems and raise levels of intracellular glutathione.
This adaptation mitigates the oxidative damage caused by chemotherapy, but inadvertently promotes drug resistance and weakens the effectiveness of treatment.
Chemotherapy may also cause a variety of adverse effects, including hepatotoxicity, cardiotoxicity and neurotoxicity.
According to the clinical practice guidelines of the Chinese Society of Clinical Oncology (CSCO) and the European Society for the Study of the Liver (EASL), liver protection therapy is recommended when alanine aminotransferase (ALT) levels exceed three times the normal value or total bilirubin exceeds twice the normal value.
The guidelines do not specify whether glutathione can be used, nor do they provide recommendations on how long it should be used, and there is no uniform standard for the use of liver drugs in clinical practice.
Previous studies have shown that elevated levels of glutathione in various tumors can lead to chemotherapy resistance and counteract the cytotoxic effects of chemotherapy.
There are currently limited studies on the effects of non-standardized glutathione intake on chemotherapy for breast cancer.
This study explored the relationship between glutathione intake and adjuvant/neoadjuvant chemotherapy resistance through a large cohort analysis of breast cancer patients.
The study also evaluated intracellular glutathione and antioxidant oxidase levels in patients receiving neoadjuvant chemotherapy, providing reference value for selecting appropriate doses of glutathione as a hepatoprotective agent.
The study collected clinicopathological data of 460 breast cancer patients who received adjuvant chemotherapy in Henan Provincial People's Hospital from January 2016 to December 2019.
Clinicopathological features were collected after glutathione treatment and compared with non-glutathione group by 1:2 propensity score matching (PSM).
The expression levels of intracellular glutathione and antioxidant enzymes (NRF2, GPX4 and SOD1) in tumor tissues of 51 patients receiving neoadjuvant chemotherapy were detected.
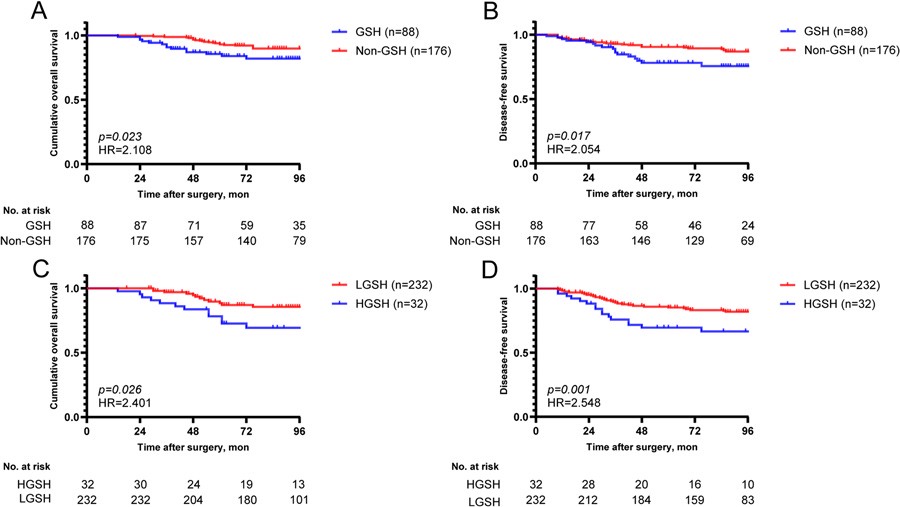
The recurrence rate after adjuvant chemotherapy was significantly higher in glutathione group (n= 28,31.8%) than in non-glutathione group (n= 39,22.2%; P=0.010).
The recurrence rate in H glutathione group (high glutathione intake, ≥16 days) was higher than that in L glutathione group (low glutathione intake, <16 days) (n=15[46.8%] vs. n=52[22.4%]; P=0.003).
Cox regression analysis showed that high glutathione intake, Ki67≥30%, triple-negative, and lymphovascular invasion were independent risk factors for disease progression after adjuvant chemotherapy.
In patients receiving neoadjuvant chemotherapy, intracellular glutathione levels and expression levels of antioxidant enzymes (NRF2, GPX4, and SOD1) were significantly higher in drug-resistant patients (P<0.001).
This study suggests that overconsumption of glutathione may contribute to chemotherapy resistance in breast cancer patients and identifies high glutathione intake as an independent risk factor for tumor recurrence.
Chemotherapy can induce tumor cells to produce glutathione to counteract oxidative damage.
These findings urge researchers and clinicians to evaluate the impact of glutathione in promoting chemotherapy resistance and to evaluate the duration of glutathione intake during treatment to optimize treatment effects.
References:
1. Zhu Zhongling, Yan Zhao. Research progress of targeting glutathione antioxidant system to reverse tumor drug resistance [J]. Chinese Oncology Clinic, 2015, 42(23): 1143-1147. (in Chinese) DOI: 10.3969/j.issn.1000-8179.2015.23.146
2. Lushchak VI. Glutathione homeostasis and functions: potential targets for medical interventions[J]. J Amino Acids, 2012, 2012: 736837.